A modern anesthesiologist has several types of labor anesthesia in his arsenal. But most often it is epidural anesthesia that is used. This choice is completely justified. Well-developed techniques, modern instruments, and the use of new local anesthetics and antimicrobial drugs for treating the skin at the puncture site make this type of anesthesia widely available and quite safe. In developed countries, epidural anesthesia is used as the main method of pain relief for both natural childbirth and caesarean section. Compared to other methods of pain relief, epidural anesthesia has a number of advantages.
Firstly, this is an effective pain-relieving method in which the woman in labor remains conscious. Secondly, epidural anesthesia has a relaxing effect on the cervix. Thirdly, in the case of uncoordinated labor, in which the muscle fibers of the uterus do not contract synchronously, it is capable of exerting a coordinating influence. Finally, epidural anesthesia, as practical observations show, has minimal effects on the child.
Mechanism of pain relief
To understand how epidural anesthesia works, a short excursion into anatomy is necessary.
As you know, the spinal cord is located in the spinal canal and is surrounded by several membranes. Nerves - the so-called spinal cord roots - stretch from the brain to other organs. The anterior roots are “responsible” for the contraction of skeletal muscles, i.e. for movement, and the rear ones for sensitivity, including pain. Nerve roots exit through the dura mater into the epidural space
, where they are surrounded on all sides by adipose tissue. It is into this space that the anesthetic substance is injected.
Note.
Sometimes
the epidural space
is called the epidural space. The words “peridural” and “epidural” are derived from the Latin dura mater - dura mater, epi - above, peri - about.
Why is a procedure affecting the part of the central nervous system - the spinal cord - relatively safe?
- The anesthesiologist's needle does not reach the spinal cord and, naturally, does not penetrate it.
- The anesthetic substance is delivered to the sensitive dorsal roots and, if it affects the anterior motor roots, it is usually insignificant (a woman giving birth usually retains the ability to move independently, although sometimes she may feel numbness in her legs - this depends on the drug used),
- An anesthetic introduced into the epidural space enters the blood very slowly. The liver manages to neutralize the medicine before its concentration in the blood becomes sensitive to the child.
What is spinal anesthesia?
Surgeries in the pelvic and leg areas, which require pain relief and at the same time maintaining the patient's consciousness, are performed under spinal anesthesia. The drug injected into the subarachnoid space acts directly on the nerve endings. In this case, a person can sometimes even move his legs, but not feel pain. Indications for the procedure:
- Surgery on the lower extremities.
- Surgical intervention on the pelvic organs.
- Surgery on the small intestine.
- C-section.
- Complicated childbirth.
If it is necessary to eliminate severe pain that occurs due to inflammation of the intervertebral discs, spinal anesthesia can also be used.
To carry out the procedure, the patient is asked to lie on his side or sit with his back to the anesthesiologist and relax his back as much as possible. The head drops as low as possible, the shoulders relax, the back should arch outward like a wheel so that the vertebrae stick out like a brush. A puncture is then made and a small amount of anesthetic is slowly injected.
To ease contractions, women in labor may also be offered anesthesia, but women are given epidural anesthesia, as it does not lead to loss of general sensitivity and muscle relaxation. With this type of anesthesia, unlike spinal anesthesia, the anesthetic is injected into the epidural space of the spine, and with spinal anesthesia - into the subarachnoid space.
Not all patients have a headache after anesthesia; many people note that there were no unpleasant sensations either during or after the operation. But there is also a percentage of patients who note the occurrence of complications:
- Pain in one leg, parts of the limb, felt for several days.
- Intense back pain.
- Feeling of heaviness and pressure on the chest, difficulty breathing.
- Pain in the neck.
- Difficulty moving the neck.
Paralysis of the lower extremities is extremely rare and only if unforeseen complications occurred during the operation, the patient was found to be allergic to the injected drug.
How is epidural anesthesia performed?
A woman sits or lies on her side, arches her back (in this position, which is sometimes compared to the pose of an angry cat, the distance between the spinous processes of the lumbar vertebrae increases - these processes protrude in the center of the back, and you can feel them yourself; in thin people they clearly visible). Before performing a puncture, the skin is treated with antibacterial treatment and anesthetized.
.
Note.
Anesthesia of the skin and subcutaneous tissue is carried out by administering an anesthetic with a separate injection using a thin needle. But, since inserting a needle into the epidural space feels comparable to a regular injection, this procedure often does not provide pain relief.
The anesthesiologist then inserts a special needle between the spinous processes of adjacent vertebrae at the lumbar level. To make sure that the needle actually entered the epidural space, the doctor performs a special test
.
Note.
The doctor pulls the plunger of the syringe towards himself, checking whether blood enters it (this can happen if the needle gets into a blood vessel) or cerebrospinal fluid (if the needle gets into the spinal canal).
Then a thin catheter is passed inside the needle to the level of those spinal cord roots that are responsible for the pain sensitivity of the abdominal and pelvic organs. After this, the needle is removed, the catheter is secured on the back with an adhesive tape and a special adapter lock is installed on it for administering drugs. The woman lies on her back. In order to check whether the catheter is installed correctly and whether the woman has an allergic reaction to the drug, a test dose of anesthetic is administered. After this, the main dose of the drug is administered. Subsequently, the painkiller is administered in portions - as pain appears or at 30-minute intervals. Each time before the administration of an anesthetic, the woman in labor is examined by an obstetrician.
A few minutes after the administration of the drug, the woman in labor begins to feel warmth and weakness in her legs, contractions become painless. If the uterus contracts ineffectively, then after the start of the procedure, normal full-fledged contractions are very often established, and the process of dilation of the cervix is accelerated. High blood pressure during epidural anesthesia is stabilized by relieving spasm from small vessels, so this method is recommended for patients with arterial hypertension, coronary artery disease and some types of heart defects, and renal failure. At a normal level of blood pressure, in order to prevent its possible decrease, the woman in labor is given an IV with solutions that are harmless to the baby and increase blood volume.
.
Note.
Maintaining the level of blood pressure in the body is ensured by vascular tone and the filling of blood vessels with blood. Since vascular tone decreases as a result of epidural anesthesia, there is only one way to maintain blood pressure - introducing an additional volume of fluid into the bloodstream.
Before the end of the first stage of labor, pain relief stops: restoration of sensitivity helps the development of normal pushing. In some countries, anesthesia is provided for the first and second stages of labor, but in Russia it is customary to anesthetize only the first stage. The fact is that under the influence of an anesthetic, the second stage of labor often lengthens, which often leads to the need for surgical intervention. Sutures are placed on the tears or incision of the perineum after the introduction of a new portion of the anesthetic. For two hours after birth, the young mother is under the supervision of an anesthesiologist and obstetrician. Before transferring the woman to the postpartum ward, the catheter is removed.
Typically, epidural anesthesia is performed during a planned cesarean section. Note that epidural anesthesia, in which the woman in labor is fully conscious at will, is carried out only until the baby is born. When doctors sew up the incision, the woman is given sleeping pills.
If a woman is afraid of surgery, she is given epidural anesthesia, after which she is given a sleeping pill before the operation begins. This does not require artificial ventilation (as with anesthesia), which means the risk of complications to the lungs is reduced. Therefore, this method of pain relief is recommended for smokers, patients with chronic bronchitis, and bronchial asthma. After the operation is completed, a solution of a narcotic drug is injected into the epidural space. As a result, the woman does not feel pain at the incision site for six to ten hours.
Note.
From the epidural space, the drug enters the blood so slowly and its concentration is so low that it has no side effect on the baby, who is applied to the breast 10-12 hours after birth. In some clinics, the baby is put to the breast immediately after birth, even before the uterus is sutured; in this case, the drug also does not have a negative effect on the baby, since it is administered after suturing.
During epidural anesthesia, as well as the day after childbirth, the woman must remain in bed.
Modern drugs used for anesthesia, as a rule, do not cause allergic reactions, have a strong analgesic effect, and are practically harmless. For vaginal delivery, short-acting drugs are used, and for caesarean section - long-acting drugs. The main drugs are short-acting lidocaine (up to 1 hour) and long-acting bupivacaine (up to 3 hours).
Marshall Klaus, doctor:
In the last decade, the number of women giving birth with epidural anesthesia has increased rapidly. The development and spread of this form of anesthesia in obstetrics gave invaluable privileges to those women who required a caesarean section, since in this case the woman was conscious and monitored what was happening.
In contrast to the general consensus on the beneficial role of epidural anesthesia during cesarean section, there are differing opinions regarding its use in the case of a healthy woman who has a favorable prognosis for normal physiological labor. Many anesthesiologists characterize epidural pain relief as the “Cadillac of anesthesia.”
They note that this is an ideal way to provide long-term pain relief to a woman while the uterus gradually opens. Sometimes slowly progressing labor is accelerated when an epidural is placed. For women who feel that they cannot bear the pain of childbirth, it is a great blessing that epidural anesthesia not only relieves pain, but also allows the woman to remain fully conscious.
Many medical publications discussing the use of the epidural evaluate it positively. In addition, word of mouth from established mothers to future mothers also votes “yes.” As a result (and taking into account the fact that many maternity hospitals and hospitals have anesthesiologists on duty 24 hours a day to staff the maternity ward), the rate of use of epidural anesthesia in some medical institutions has exceeded 90%.
Contraindications and complications
Epidural anesthesia is unacceptable in cases of unconsciousness or eclampsia
, bleeding disorders, purulent lesions of the skin of the back, general blood poisoning (sepsis), injuries to the brain and spinal cord, spine, high intracranial pressure, migraines, allergic reactions to the anesthetic used.
Note.
Eclampsia is a severe form of gestosis, accompanied by life-threatening disorders: convulsions, arterial hypertension, loss of consciousness.
Relative contraindications are curvature of the spine and diseases of the nervous system. In these cases, the doctor makes a decision about anesthesia based on the specific situation.
Sometimes complications may occur during and after epidural anesthesia:
- Headache. It usually appears on the first to third day after birth as a result of damage to the dura mater and leakage of cerebrospinal fluid into the epidural space. The pain may last for 1-2 weeks, sometimes lasting up to 6 weeks. Treatment usually includes bed rest, sedatives, painkillers, and caffeine.
- If the sterility of the manipulation is violated, inflammation at the injection site, epidural space, and the membranes of the spinal cord and brain is possible.
- When the main dose of the drug is administered instead of the epidural space into the spinal canal, the patient may temporarily lose the ability to move. This condition lasts only for the duration of the drug's effect.
- When the main dose of anesthetic is introduced into a blood vessel, a sharp drop in blood pressure and disruption of the heart may occur.
- Manifestations of allergic reactions to the drug used.
When anesthesia is administered correctly, complications are rare. It should be said that special scientific studies of the effect of epidural anesthesia on a child have not been conducted, but practical experience shows that the effect of epidural anesthesia on a child is minimal. However, with the development of complications, such as a pronounced drop in blood pressure, placental circulation may be disrupted.
In conclusion, I would like to say that labor pain is a sensation that allows a woman to navigate what is happening to her and act as necessary at the moment of childbirth. It should be said that the sensitivity threshold is different for different people, and accordingly, women experience the process of childbirth differently. Normal mild labor pain does not require pain relief (as you would not want to use anesthesia to relieve pain after strenuous exercise). Fear of pain is the real psychological cause of a vicious circle in which pain causes fear, and fear increases pain. This often causes disruption of labor. It is only in cases where the pain is so severe that it overpowers all other sensations, or when the use of anesthesia is mandatory (for example, during a caesarean section), intervention by anesthesiologists is really necessary.
Dmitry Ivanchin Anesthesiologist-resuscitator, senior doctor of the operational department of the Center for Emergency Medical Care of the Moscow Health Committee.
What do American anesthesiologists say about epidural anesthesia?
Recently, a page appeared on the American Society of Anesthesiologists website about common “myths” about epidural anesthesia.
Anesthesiologist Paloma Toledo studies the issue of medical pain management during childbirth and also chose this type of pain management for her birth. Below we provide a translation of this page. It is interesting that not a single link to the study is attached to the refutations of the myths. We don’t even know why exactly anesthesiologists in the mass media insist on the safety of epidural anesthesia for childbirth, while midwives and doctors who are not directly interested in distributing the service are more wary of epidural anesthesia.
Not so long ago, a book by an American anesthesiologist was even published, “Epidural anesthesia without guilt. Childbirth without pain,” which caused a lot of noise.
We decided to add small comments to the translation with links to sources.
picture
Myth 1: An epidural slows down labor.
There is no reliable evidence that epidurals (or other pain relief procedures) slow down labor.
Because epidurals are most often used for “difficult” births as opposed to easy ones, some have chosen to present the message as saying that it is the epidural that makes labor difficult. This is a misinterpretation of the data. On the contrary, there is some evidence that an epidural may actually speed up labor for some women, allowing them to relax.
Now we can say that pain relief does not have a significant effect on the process of childbirth.
Comment from Très bébé Class:
One of the most comprehensive medical research databases, the Cochrane Collaboration, has reverse information. A review of epidural anesthesia during labor noted that at least the second stage of labor (=pushing) was longer in women who used this type of pain relief. The slowdown in labor is also indicated by the fact that women are more likely to receive stimulation during labor with epidural anesthesia.
By the way, almost all studies compare not women with epidural anesthesia and no pain relief at all, but women with epidural anesthesia and women with narcotic pain relief.
Nerve endings in the cervix, and then the muscles of the pelvic floor and vagina, transmit signals about tissue stretching, in response to which the pituitary gland produces more and more oxytocin, which increases the rate of labor. Numbness of the nerves caused by epidural anesthesia may be due to the labor slowing effect of this type of analgesia (adapted from Henci Goer).
On the other hand, it is true that epidural anesthesia may be useful if a woman becomes very tense during contractions and is unable to cope with the pain. In this case, an epidural can actually help with dilatation.
Myth 2: An epidural leads to a Caesarean section birth.
Again, there is not enough evidence that epidurals cause caesarean section births. Women who receive an epidural report more pain than those who do not receive this type of pain relief. Such pain itself may be a marker of an unusual labor, which may last longer or end in a caesarean section. Women who request an epidural often dilate more slowly than usual, they give birth to larger babies, they are more likely to be induced in labor, and it is often their first birth.
Comment from Très bébé Class:
Indeed, there is no sufficient evidence yet, but research is already underway. For example, an association has been found between the use of epidural anesthesia and the number of births by caesarean section. Where doctors used this type of pain relief on fewer than 40% of women, the C-section rate was about 10%. In contrast, where the rate of epidural anesthesia during labor was 71-100%, the rate of cesarean sections was 23.4%.
An association has also been found between posterior positioning and the use of epidural anesthesia. However, it is really not yet clear how they are interconnected. Since childbirth from this position usually lasts longer and is more painful for the mother.
It is worth adding that epidural anesthesia, while reducing pain, increases the risk of using a vacuum extractor, and, accordingly, the risk of serious damage to the perineal tissue. These injuries can cause women significant discomfort in the first days and weeks after childbirth.
Myth 3: You can't get an epidural until you're dilated to a certain level.
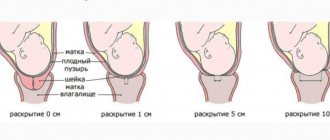
Women should not wait until they are dilated to a certain level before asking for an epidural. According to American Society of Anesthesiologists protocols, “patients are offered regional anesthesia (spinal or epidural) during the latent phase of labor, if this service is available, without being bound to arbitrary standards of cervical dilatation.” If a woman in active labor feels uncomfortable, an epidural is the most effective method for pain relief. There is no medical reason to wait until your cervix is dilated to a certain point.
Comment from Très bébé Class:
Studies (for example, here and here) show that the timing of epidural anesthesia may still be important.
The study found. that the provision of epidural anesthesia before 4 cm of dilation does not affect the progress of labor was carried out in a comparison of two groups of women: some were given epidural anesthesia immediately as they asked (even if the dilation was less than 4 cm), others were first given a narcotic analgesic, and then, after 4 cm , - epidural anesthesia. In the first group, 18% of births were by cesarean section, while in the second group it was 21%.
However, there is no comparison with a group of women without medical analgesia.
Myth 4: Women with lower back tattoos cannot get an epidural.
There is no evidence that lower back tattoos cause harm in this situation. Giving an epidural through tattoo ink will not introduce ink into the bloodstream or spinal canal or cause subsequent complications to either mother or baby.
Comment from Très bébé Class:
There is a feeling that this myth is here only to set off other more weighty arguments with its absurdity).
Myth 5: Epidurals are incredibly painful.
For most patients, the most painful part of getting an epidural is freezing the area in the lower back before the catheter is inserted, which actually causes a burning or tingling sensation. The insertion of the epidural catheter usually feels just like pressure. For a few hours or days after giving birth, some women feel discomfort in the lower back where the needle was inserted, but this rarely becomes a problem.
Comment from Très bébé Class:
Here the pain from the anesthesia and the discomfort afterwards were somehow mixed together.
After the study they say this: severe headaches for several days - in 0.1% of women, chronic pain (weeks/years) in the back (18.2% of cases with anesthesia and 10.2% of cases without it), headaches (4.6% of cases with anesthesia and 2.9% of cases without it), migraine (1.9% with anesthesia and 1.1% without it).
Myth 6: Epidural anesthesia can cause permanent medical problems for the mother and/or newborn.
Serious complications from epidural anesthesia are extremely rare. The biggest risk patients face is that the epidural may not work as effectively as desired. In such cases, the anesthesiologist may increase the dose of the drug or make other adjustments.
Comment from Très bébé Class:
Indeed, serious irreversible complications (convulsions, heart attack, respiratory paralysis and allergic shock) are extremely rare.
Myth 7: An epidural makes childbirth a less satisfying experience for a woman.
What makes a meaningful and satisfying birth is subjective, but the important thing for most women is to remain vigilant, aware of contractions, and involved in the birthing process. An epidural does not interfere with any of these things. Eliminating the distracting pain of labor can make the birthing experience more enjoyable for many women.
Comment from Très bébé Class:
We have already written about research into what makes childbirth a satisfying experience for a woman. It’s great when a woman feels supported during childbirth and has the opportunity to participate in decision-making without pressure in one direction or another (give birth without anesthesia/take immediate pain relief).
But the fact that a woman who refuses pain relief is often perceived as masochistic, “overly heroic,” uninformed and “zombified” is not yet known.
Pain, which performs an important function as a means of feedback during childbirth, is perceived as a danger, and epidural anesthesia, on the contrary, as a benefit necessary for everyone. At the same time, the woman’s body prepares for pain and responds to it: by the time a child is born, a woman’s blood contains 30 times higher levels of endorphins (natural analogues of opiates) than a non-pregnant woman. For those who have had a long and difficult birth, the level of endorphins rises even higher. (based on materials from Henci Goer)
Myth 8: Epidural anesthesia makes the baby sluggish and interferes with breastfeeding.
Some women worry that the medicine they are receiving may somehow transfer to the baby and make it less able to breastfeed. Since learning to breastfeed is not always easy, most maternity hospitals have “lactation specialists” who help mothers and newborns practice this skill. An epidural actually exposes your baby to the least amount of medication compared to other pain management methods.
Comment from Très bébé Class:
Here again a very elegant substitution of concepts occurs. Indeed, compared to narcotic analgesics, epidural anesthesia exposes the baby to the least amount of drug exposure, and a lactation consultant can be called to the maternity hospital and try to solve problems associated with lactation.
However, this does not invalidate research that shows that epidural anesthesia during labor is associated with later difficulties in breastfeeding.
Myth 9: There is a temporary window for epidural anesthesia and it can close.
The main requirement for epidural anesthesia is that the patient can sit still and the baby has not yet been born. Apart from this, there is no mandatory time when it is “too late” for the procedure.
Comment from Très bébé Class:
Doctors usually offer epidural anesthesia when the dilation is from 4 cm to 7 cm. They don’t do it earlier because of the risk that contractions will become less frequent; later, because the woman’s individual sensitivity is unknown and there is a high probability of being in a situation where it’s time to push, but the woman doesn’t feels nothing. In Russia, it is customary to remove epidural anesthesia before pushing, but this is not done all over the world. Some studies show that removing anesthesia for pushing does not reduce the number of side effects (use of forceps and vacuum extractor).
Myth 10: An epidural will guarantee optimal relief.
As with any medical procedure, each person reacts differently to medications and sometimes not enough medication is given in the right place. These cases are rare and when they occur, the anesthesiologist can make adjustments.
Comment from Très bébé Class:
We have nothing to add here. Is it about the funny (but not for a mother in labor, of course) domino effect, when only one half of the body is anesthetized.
Read about what to do if you already have an epidural.
Learn how epidural anesthesia works here.
Does epidural anesthesia during childbirth hurt?
Fear of the unknown is always present. This is one of the reasons why women agree to use medications to eliminate or reduce labor pain. Epidural anesthesia is considered the safest medical method to cope with this task.
Regional administration of drugs into the space near the spine allows the woman to remain conscious and not feel contractions.
But is it painful to have epidural anesthesia during childbirth, what is the manipulation and what are its consequences - these are the doubts that are present in the head of every pregnant woman.